Millions of Americans depend on small, rural hospitals for healthcare. Unfortunately, due to several challenges, many of these small hospitals are struggling to survive.
Between 2010 and 2014, 47 rural hospitals across America stopped providing inpatient services, according to a report by the Rural Health Research Gateway. An additional 673 rural hospitals are at-risk for closure.
Today’s climate may seem daunting for small, rural hospitals – but it doesn’t have to be. Today, we’re highlighting some of the best strategies today’s small, rural hospitals are using to survive.
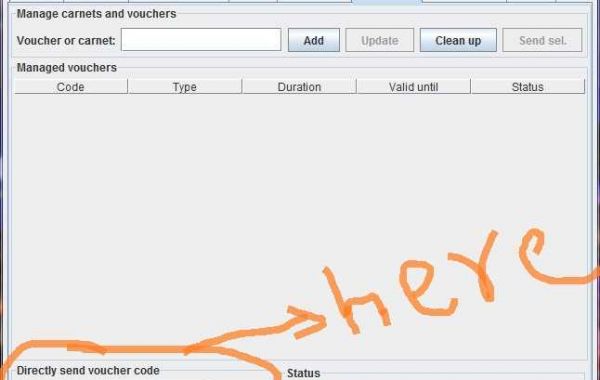
Conduct Top-to-Bottom Financial Analyses, Audits, and Assessments
Good hospital management starts with good data. One of the smartest things a small hospital can do is to conduct a 360-degree financial analysis using at least five years’ worth of data.
An objective third party – like HMI LLC or other medical consulting organizations – can pore over the data to issue concrete recommendations. You can see how your hospital compares to other organizations with a similar size and market.
Financial audits can reveal surprising problems with smaller, rural hospitals, including:
• Revenue cycle services issues
• Denials management issues
• Longer lengths of stays compared to other hospitals
• Outdated systems still in use
• Medical coding compliance issues
• Billing and purchasing problems
A top-to-bottom financial analysis can show a small, rural hospital what they’re billing and buying and how the hospital is doing it. It can identify key problems at every stage of the organization, including areas of missed revenue expectations, the best areas of potential improvement, and actionable changes the organization can implement today.
Implement Better Debt Management
Many of America’s small, rural hospitals are at risk because of outstanding debts. If the hospital can learn to effectively manage this debt, it can be the difference between surviving and shutting down.
Debt management strategies vary between organizations but can include all of the following:
Judicial Reorganization: Judicial reorganization is a bankruptcy handled through the court. There are pros and cons to this type of debt management. Reorganizations can trigger default on bonds, making them due immediately, for example. Bankruptcy can also lead to the loss of revenue streams from CMS and other payors. However, for some small hospitals in certain situations, it’s the best path forward.
Debt Structure Refinancing: Refinancing hospital debt may be a smart option when interest rates are low or a hospital’s credit rating improves. However, it’s not the right choice for all hospitals in all situations.
Non-Judicial Reorganization: With non-judicial reorganization, hospitals restructure their debt and payment plans with debtors outside of the court. Good reorganization can create additional time for the small hospital without resorting to bankruptcy.
Selling: Putting a hospital on the market is one option for smaller hospitals overwhelmed by debt. This option can be particularly challenging, as larger systems will naturally absorb the patient flow after a hospital closes even if they don’t buy the facility.
Identify New Revenue Streams
Generating new revenue is a great way to revitalize any business. With smaller hospitals, it’s easier said than done. However, small hospitals that want to become financially sustainable will need to develop new revenue sources – especially the hospitals that cannot cut or refinance their way to a solution.
One of the most common ways for small, rural hospitals to create new revenue is by teaming up with outpatient healthcare providers. A smaller hospital can make its facility available to the group and setup a revenue sharing program.
Many hospitals have successfully setup behavior health programs, for example, because Medicare and Medicaid now cover behavioral health services. It’s a new revenue stream that also provides a valuable service to the community.
Increase Residency Programs and Partnerships
There are approximately 80 primary care physicians (PCPs) per 100,000 people in the United States, although there are only 68 PCPs per 100,000 people in rural areas.
With that in mind, many smaller hospitals have achieved success by increasing residency programs and partnerships. It’s not just about training new doctors: it’s about keeping them long-term.
Here’s how one report explained the benefits of better rural residency programs:
“Medical residents who train in rural settings are two to three times more likely to practice in a rural area; especially those who participate in rural training tracks.”
Implement Telehealth Services
Smaller, rural hospitals may not have specialists on-site for every patient’s needs. That’s why a growing number of smaller hospitals are using telehealth to fill the gaps.
Telehealth can fill the gaps in subspecialist care, eliminating the need for patients to travel long distances to see a qualified healthcare provider.
Telepharmacy is one growing area of telehealth. Telepharmacy gives patients the convenience of remote drug therapy monitoring and authorization for prescriptions. Patients can also remotely access pharmacy counseling to maintain compliance with prescriptions.
There’s also telepsychiatry, which provides behavioral health services to patients who would otherwise have to drive hours to see a mental health provider.
Build Hospital Loyalty
Most people prefer to shop local. Just like a small business, a small hospital must build brand loyalty with the community.
By strengthening ties with consumers, physicians, and the local community, hospitals can keep their brand in the front of patient’s minds. Create a hospital-branded mobile app, for example, or sponsor local events.
Eliminate Waste and Redundancy at All Stages
Smaller, rural hospitals don’t have the resources of larger providers, so they need to compete in other ways.
An in-depth consultation or assessment can reveal surprising insight into missed revenue opportunities and inefficiencies within a hospital.
Some smaller hospitals have long wait times, which means patients are turned away and forced to visit other providers, leading to lost revenue every year.
Other hospitals have inefficient or outdated systems, increasing the number of steps taken before every treatment.
By eliminating steps in payroll processing, contract management, and other organizational systems, hospitals can save time and money, leading to lower costs and better patient care.
Final Word
Hundreds of small, rural hospitals across America are at risk of shutting down. However, even hospitals teetering on the edge of bankruptcy or closure can change their course by implementing smart solutions today.
Contact HMI LLC to discover the best options available to your small, rural hospital. Our team has combined decades of experience solving complex problems for medical providers across America.
Visit https://hmi-corp.com/the-best-strategies-small-rural-hospitals-are-using-to-survive/